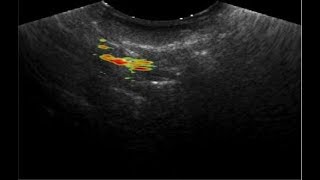
Roasted barley as a human subject swallows it over the course of 1.2 seconds.
Study: Barley May Be Next Great Medical Imaging Drink
Published July 18, 2018 This content is archived.
story based on news release by cory nealon
Jacobs School of Medicine and Biomedical Sciences researchers have found barley may be used as an edible contrast agent to show doctors what’s happening inside their patients’ bodies.
The researchers studied more than 200 types of tea, chocolate, herbs and other foodstuffs before finding that roasted barley — when struck by a common laser — can illuminate the throat and gastrointestinal tract.
New Medical Use for a Common Grain
The discovery could improve physicians’ ability to diagnose swallowing disorders, which affect more than 15 million Americans, as well as gut disorders.
What’s more, because many human diets already include barley, it could be fast-tracked for medical use.
“It’s really incredible. Here you have this common grain — it has been grown all over the world for thousands of years, and used to make tea, bread, beer — and we’re just now finding another use for it as a contrast agent for medical imaging,” says Jun Xia, PhD, assistant professor of biomedical engineering, which is a joint program between the Jacobs School and UB’s School of Engineering and Applied Sciences.
Xia and 10 other UB co-authors described the experiment and its results in a study, titled “Ingestible Roasted Barley for Contrast-Enhanced Photoacoustic Imaging in Animal and Human Subjects,” published in May in the journal Biomaterials.
Emerging Alternative to Barium
Swallowing disorders, also known as dysphagia, can be an indication of a serious medical problem. They are caused by everything from cancer and Alzheimer’s disease to missing teeth and neck injuries.
To test for dysphagia, doctors typically have patients drink a thick, chalky liquid called barium. Doctors then use X-rays, MRIs or ultrasounds to look inside the throat. Each technique is limited with respect to safety, high-cost and lack of adequate contrast, respectively.
Photoacoustic computed tomography (PACT) is an emerging alternative.
Like barium, patients drink or are injected with a contrast agent — often newly developed nanoparticles made of metals, polymers and other materials. A laser strikes the nanoparticles, generating pressure waves that can provide nuanced and real-time views inside the body.
Study Focused on Dark Food, Beverages
One drawback to contrast-enhanced PACT is the often lengthy and expensive regulatory process for new contrast agents.
“That’s what led us to search for edible alternatives. Because we’ve been eating or drinking these products, we know they’re safe for most people,” says study co-author Jonathan F. Lovell, PhD, associate professor of biomedical engineering.
The researchers focused on dark foods and beverages because the darker the color, the more the foodstuff will absorb wavelengths from the laser and, theoretically, produce a clearer image.
Potential Use for Diagnosing GI Tract Disorders
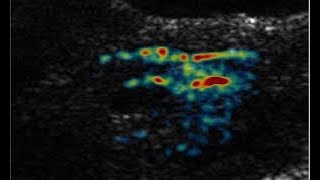
Roasted barley, a grain used to produce beer, bread and other products, provided the best results. Researchers were able to detect individual particles of it through 3.5 centimeters of chicken breast tissue, as well as through human hands.
Roasted barley tea — a drink common throughout Asia — was detectable through 2.5 centimeters of chicken breast. It worked in human subjects as well, providing visualizations inside the human throat when swallowing.
In addition to swallowing imaging, researchers say roasted barley could potentially be used to diagnose gastrointestinal tract disorders.
NIH, CTSI Among Project Funding Sources
Grants from the National Institutes of Health, UB’s Clinical and Translational Science Institute and the UB Office of the Vice President for Research and Economic Development supported the research.
Co-authors from the Department of Biomedical Engineering are:
- Upendra Chitgupi
- Jumin Geng
- Haoyuan Huang
- Dong Hyeun Lee
- Rachel Su Ann Lim
- Tri Quang Vu
- Depeng Wang, PhD
Other co-authors from UB’s School of Engineering and Applied Sciences are:
- Maggie Liu, staff assistant
- Nikhila Nyayapathi, a student in the Department of Electrical Engineering