Hands-On Research Experience
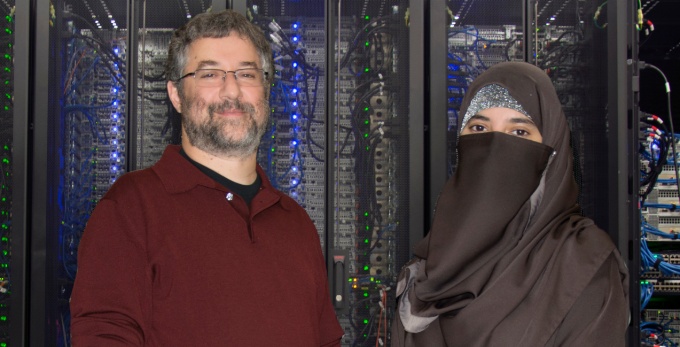
Professor Marc S. Halfon, PhD (left), has helped students — like Hasiba Asma, from another Jacobs School program — learn key bioinformatics techniques. He’s one of the mentors ready to guide you in our BRIGHT program.
We enable you to undertake a hands-on research project that’s sure to fuel your passion for a career in biomedical informatics and data science.
In our BRIGHT short-term program, we place a strong emphasis on research experience for undergraduates and master’s students.
By immersing you in bona fide research projects, we’re providing you with an excellent opportunity to experience and understand how biomedical informatics research can impact real-life health care and clinical outcomes for patients.
As a trainee in our program, you will have a specific mentor who will work with you as you complete a project over the summer. We’ll encourage you to submit an abstract to a national conference.
What Kind of Research Can I Do?
There are many possible ways to engage in research that enriches your experience in our BRIGHT program.
Examples of mentored projects include:
- Improved interoperability: Projects aim to reduce redundancies in emergency department (ED) use due to lack of EHR interoperability. We are evaluating ED utilization in patients receiving care at more than one health care institution with differing electronic health record (EHR) systems.
- COVID-19: Projects study leukotriene use and COVID-19 outcomes; vitamin D deficiency and COVID-19 outcomes; new diagnoses people have after a bout of COVID-19; and using the Computational Analysis of Novel Drug Opportunities (CANDO) therapeutic discovery, repurposing and design platform to make predictions against COVID-19.
- Ebola virus in silico tests: Integrating in vitro and multiple target inhibition in silico approaches, we select and prioritize compounds for additional in vivo testing. We use a combination of the CANDO platform and in vitro hits to identify common leads that inhibit multiple protein targets.
- Changing electronic medical record (EMR) vendors: The functionalities required of EMRs are dictated by their intended clinical domains, but currently, many EMRs fall short of those needs. We could look at factors driving changes, such as outdated technology, health system consolidation, EMR designs of one-size-fits all, and proprietary data and database structures leading to roadblocks for interoperability and data exchange.
- EHRs and poor communications at discharge: Communication and collaboration of care team members across the health care continuum are critical to positive patient outcomes after hospital discharges. Poor coordination at these times can result in rapid readmission and adverse events during and after discharge. This project develops a system architecture map to guide future development and external funding of HIT solutions to remove existing barriers, resulting in more effective transitions and improved patient outcomes.
- Natural Language Processing (NLP) to enhance structured data in identifying Nonvalvular Atrial Fibrillation (NVAF) patients and their stroke and bleed risk: Based on risk factors for stroke, therapeutic options for NVAF include low-dose aspirin or an oral anticoagulant (OAC). But OACs predispose the person to hemorrhagic side effects. This project compares clinician-rated stroke and bleed risk assessments in NVAF patient with assessments utilizing existing secondary EHR data to determine if utilizing unstructured EHR data through NLP techniques will enhance structured EHR data and improve the ability of the EHR to identify NVAF patients and more accurately assess their stroke and bleed risk.
- Rapid and de-identified research from an observational data warehouse: We create an environment to allow rapid and de-identified research from an observational data warehouse in OMOP/OHDSI and i2b2 augmented with semantic information extracted from clinical text (i.e., free text notes and reports) using relational structures, NOSQL structures and graph databases.
- Creation and validation of an automated IRB review: Investigators who believe that their protocol is minimal risk will enter data both in our system and send their application to the IRB in the usual manner. The system, which is blinded to the IRB review, will determine if the protocol is exempt, approved expedited (minimal risk) or needs a full IRB review. In this multi-center trial, we compare the judgments of the computer system to the IRB review to see if moving to an automated approach for this subset of studies would be safe.