Research by faculty members of the Jacobs School helps surgeons better prepare for delicate, life-saving surgeries.
Researchers Aim to Advance Surgery With 3D Printing
Published April 16, 2019 This content is archived.
story based on news release by gina marie ciappina
Researchers have developed a way to generate 3D prints of the human vascular system, giving surgeons pre-surgical, hands-on access to individual patients’ life-threatening vascular diseases in the heart and brain.
The 3D printing method — initiated by Ciprian N. Ionita, PhD, assistant professor of biomedical engineering, and Adnan Siddiqui, MD, PhD, professor of neurosurgery — is already being used to better prepare doctors performing delicate surgeries to treat conditions such as stroke, aneurysms, cardiac arrest and congestive heart failure.
Unparalleled Tool to Replicate Patient Anatomy
“The whole idea of these 3D-printed models is to not only mimic patient anatomy, but to also mimic some of their vascular mechanical properties,” says Ionita.
The number of models and their specifics suitable for 3D printing are endless, and they can be custom-made to fit individual patients.
“There is no better tool than 3D printing to replicate patient anatomy,” says Ionita. He predicts that 3D printing will become standard in all medical fields in the near future. As of now, radiology departments across the country are adopting 3D printing as a new 3D medical imaging representation, he says.
Due to increased acceptance, 3D printing will become a reimbursable tool as of June 2019, allowing doctors to use it as a patient service for better diagnosis and treatment planning for high-risk patients.
Ionita explains the main goal of this 3D printing is to create major advancements in surgery through biomedical engineering and diligent teamwork.
From the moment a patient arrives at the hospital, to the analysis of post-surgery for research purposes, the entire team works together to correct the patient’s life-threatening vascular condition.
“We as a team hope to achieve safer surgery with less complications,” he says, “and ultimately save lives.”
Models Help Train Residents and Students
The 3D models are being used to train residents and medical students learning how to proceed with delicate and often life-or-death procedures.
The prints are available at the Gates Vascular Institute for those in training to learn the proper methods for treating vascular conditions.
Ionita says students receive a better education by witnessing the decision-making process all the way from a patient scan to surgery. “Without human interrelation between the researchers and the surgeons,” says Ionita, “the meaningful medical work can’t be done.”
Additionally, graduate students use the models for research.
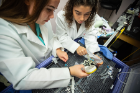
Lauren Shepard and Kelsey Sommer, two students in the biomedical engineering doctoral program and Ionita’s student assistants, study how to use the 3D prints to better understand the flow and pressure conditions within a patient’s diseased arteries. In one particular experiment, Shepard is trying to understand how different variants in the brain vasculature affect the pressure gradients and flow.
Helping Surgeons With High-Risk Cases
“We are trying to help surgeons who have really difficult cases and have doubts about the approach,” says Ionita. “They will then have us make a model, come to the lab for surgical planning and practicing and make a decision.”
When treating a patient with a very high-risk or novel procedure, a doctor and his team head to Ionita’s lab. This is where they practice on the patient-specific model to develop a customized surgical plan. How they want to approach the model will determine their steps. If it does not work on the model, Ionita says, they will then readjust the surgeon’s plan and keep track of the changes.
“There was a case where a surgeon made changes to 70 percent of the steps he was going to do originally,” says Ionita. The surgeon decided to use different devices and stiffer wire to better accommodate the patient during surgery, based on the outcome of practicing the surgical plan on the model.
Database Can Enable Important Work
Soon there will be an extensive database of brain and heart vascular scans compiled in clinical trials. In addition to the models making it easier for doctors to decide what surgical tactics to take, this large database can speed up testing for a new device or a procedure used in the clinic.
“The whole idea is for us to understand more depth into a patient’s vascular structures’ interaction with the devices and blood flow, why a person would fully recover from an aneurysm after six months and why another patient would not,” says Ionita.
“At the end of the day, it’s about a patient’s specific geometry and vascular mechanics, which make the difference between two patients.”
Printing Process Comprised of Multiple Phases
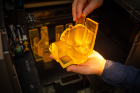
The 3D-printed models are built to scale for a patient’s arteries, and are often referred to as “phantoms.” The models are warmed up during surgical practice sessions to simulate the elasticity of arteries within a vascular system and to allow the devices, fabricated with shape memory alloys, to behave the same as in human arteries.
The first phase of the process starts when a patient receives a diagnosis from a doctor, Ionita explains. “They give us problems,” he says, “then we try to solve them.”
Next, a scan of the diseased area is taken through 3D medical imaging.
A process called segmentation — or the selection and isolation of the structure of interest — is collected and analyzed. Once a specific segment is located, engineers create a 3D geometry and put it into a secondary software to manipulate before printing the model.
The model, or phantom, is then in-house 3D printed. Depending on the patient, the print can be used to understand hemodynamics, validate medical software, test devices or create a surgical plan.
In the final phase of the process, the surgical team starts surgery by using the approach they perfected on the patient-personalized model.
Complexity and Materials Dictate Print Time
A model can take from 20 minutes to 20 hours to print, depending on how complex and precise the phantom needs to be, Ionita says.
The printing time also depends on the different types of material being used. Materials can be combined for a single print to get the correct texture. Rubber silicone mimics blood vessels the best and is used the most for prints, he says.
Before 3D printing, these lifelike models were costly, complicated to make and had to be shipped from Switzerland at a cost of more than $12,000 each. Now, each model costs about $100.
Replicating Study With Patient-Specific Models
Ionita’s team of biomedical engineers has worked to understand how variants of the circle of Willis — a vascular structure at the bottom of the skull that connects the anterior circulation to the posterior circulation — affects the blood in the vessels leading to the brain. The team has also worked to determine the metrics of patients’ risk level when they come into the hospital, which is extremely important for classifications.
In the cardiac equivalent of the aforementioned study, led by Sommer, the researchers examined how catheter lab measurements of pressure gradients across coronary arteries correlate with measurements in the lab. The study was conducted in collaboration with Vijay S. Iyer MD, PhD, clinical associate professor of medicine, and Michael F. Wilson, MD, professor emeritus of medicine.
“This is the first clinical trial of its own where they’re trying to replicate a study in humans with 3D-printed, patient-specific benchtop models,” says Ionita. “We concluded this cardiovascular study because we found significant correlation between the measures of flow from the model to the measures of flow from patients.”
Ionita’s team is now moving toward the neuro-application of this study and building off of what it learned in the coronary and cardiac application.
Downtown Campus Facilitates Partnerships
The Buffalo Niagara Medical Campus, home of the new Jacobs School of Medicine and Biomedical Sciences building, is a hub for medical education, research and health care.
Ionita and Siddiqui began their 3D-printing research when the Clinical and Translational Research Center, Gates Vascular Institute and Jacobs Institute were created to place engineers, physicists and vascular surgeons all under one roof.
“We are now able to optimize our research by meeting every day and working together,” Ionita says.
To enhance the mechanics of the models and make them even more lifelike, he is also working with engineers at UB’s New York State Center of Excellence in Bioinformatics and Life Sciences.